The Atlas and Axis bones are 2 of the most distinct bones in the spine. Also the first and second bones of the neck so they are often referred to as C1 and C2. And since they lie just below the skull and the Atlas, like the Greek Titan, supports the skull, this part of the body is called the craniovertebral junction or CVJ.

The skull ends in a large hole called foramen magnum (latin for large hole, I’m not kidding). The brain stem continues out of this hole to become the spinal cord. And since both structurally and functionally the spinal cord is an extension of the brain, these 2 are collectively considered the Central Nervous System (back to basics here). Along with the spinal cord and a couple of nerves, the other important structure passing through the foramen is the vertebral artery, one on each side. Why is it important, because they are the other source of blood supply to the brain. The primary source being the pair of Carotid arteries in the front of the neck.
The skull sits on top of the Atlas, and the joints between the two bones allow for nodding movements, like for “yes”.
Wiki has a lovely 3D rendering of the Atlas that allows for free movement. Knock yourselves out.
As is apparent, the atlas is otherwise a fairly thin bone barring the large ‘lateral mass’ on either side to transmit the weight of the skull to the rest of the cervical spine. You will notice 2 small holes in the far side of the bone, and these transmit the vertebral arteries.
The next bone in the series is the Axis. It is the axis around which the head rotates. It is a broad stout bone with a peg like projection called the dens or the odontoid process. The dens fits into a groove in the atlas and held there by a ligament. Which I think is the most vital ligament in the body, more on this in just a bit). This joint between the dens and the atlas is the joint that allows for rotation on the head to either side. Try it. Learn to say no.
The transverse ligament holds the dens to the atlas. This becomes important when we consider what happens when we bend our heads and necks down.
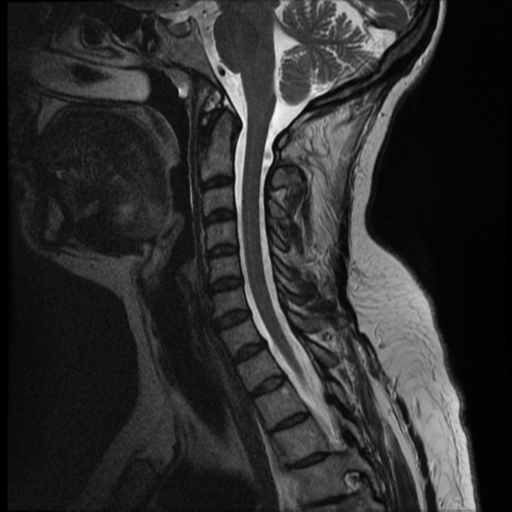
As we can see in the MRI the Spinal cord runs behind the dens and if the atlas moved independently of the dens then it would project backwards and impinge on the spinal cord. Which is not a good idea.
This is prevented by the transverse atlantal ligament. And since preventing compression of the upper most part of the cervical spine, which can lead to paralysis, respiratory failure, death even, is vital to life, I dub this the most imporant ligament.
The C1 C2 region is often the stuff of nightmares for a neurosurgeon. It can be congenitally deformed and anamolous. (I’ve dealt with a 2 year old that had spinal cord compression and dislocation of the bones). It is often damaged in high impact trauma, with some disastrous consequences (like the paralysis/respiratory failure), and sometimes just can present after trauma with unrelenting pain due to an instability. The joints can be damaged by tumors, tuberculosis and rheumatoid arthritis to name a few.
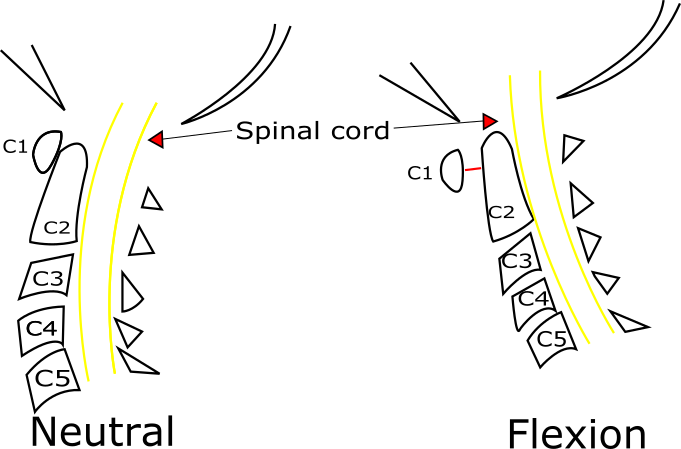
The nightmare part is in both diagnosis, since oftentimes MRIs may look normal. The true picture of instability shows up on bending Xrays which are taken with the head bent forward and then with the head extended backwards. And bony injury can sometimes be seen more clearly with a CT scan. It is also important to tell patients why so much imaging is required. The MRI shows us nerves, the CT shows bony anatomy and a dynamic Xray will show how the bones interact with each other during movement.
The case below is of a 17 year old who came to me about a month or so after a fall from a height with severe pain and restriction of movements of the neck. He had no weakness or tingling or any symptoms or signs that would suggest a spinal cord injury. He had been evaluated with an MRI which was reported as normal and looked mostly innocuous. A CT Scan and an Xray revealed a more insidious problem that needed fixing.
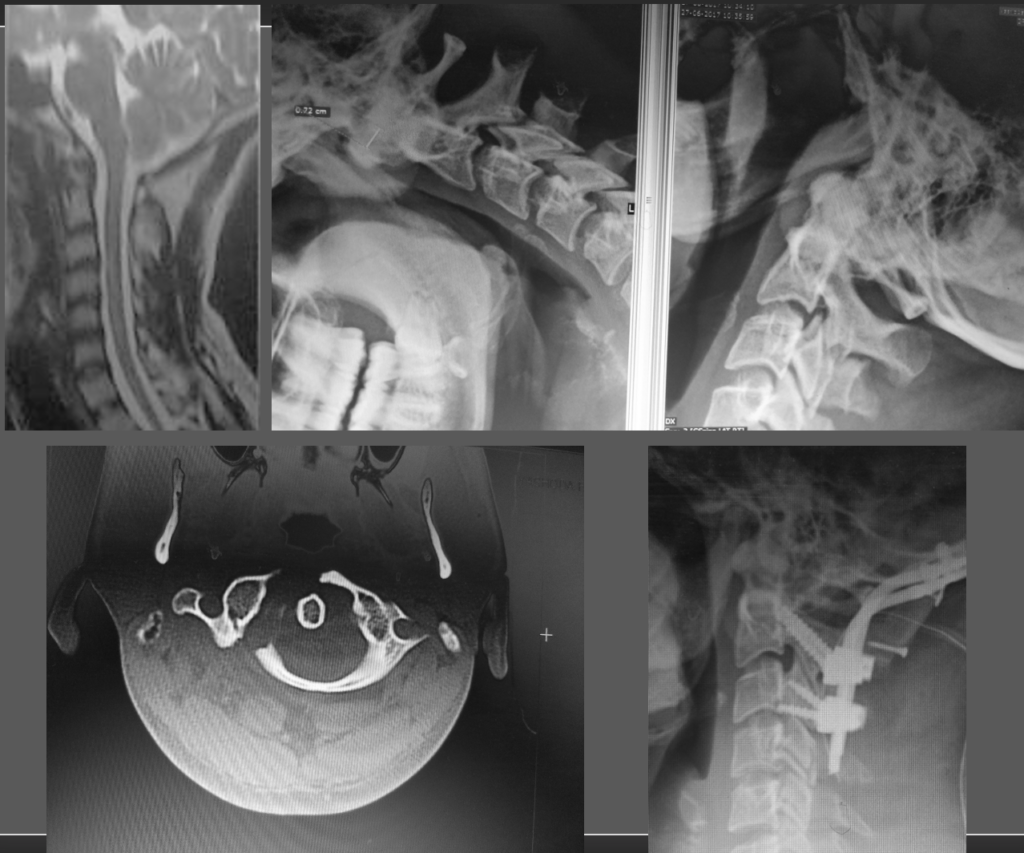
And this is just the tip of iceberg of some of the fixations that I have seen. More extensive surgeries for more difficult problems have been both described and done. at this point I would want to go back to anatomy for one small moment to highlight exactly why this part of the body is a surgical challenge.
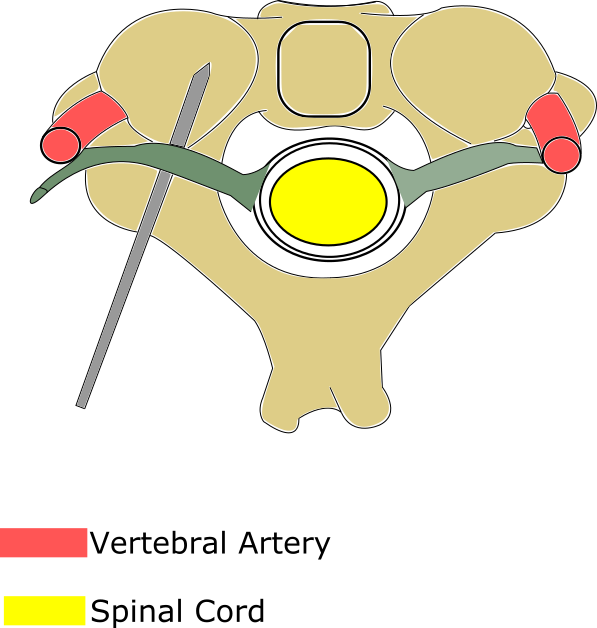
The image above (made with Inkscape by yours truly. I cannot recommend this and Vectornator enough for creating line diagrams for medical illustration) shows that the screws we need to place to fix this bone runs in 4-5mm of space with the spinal cord on one side and the vertebral artery on the other. Above is this the C2 nerve root that supplies the back of the head. Oh and the screw is usually a 3.5mm screw. Oh and till recently this was done blind. In the sense, a typical entry point was identified and with firm yet careful drilling a path would be created with constant verification by feel that no breach of the bone had occured.
As one felt the years fly past from ones life expectancy, the path for the screw was made and an appropriately sized screw placed. And then this as repeated on the other side and in C1. There are variations of the screw trajectory with slightly altering risks of damage to vital structures but the most difficult one has the best biomechanical stability.
Navigation has changed it all. I have spoken of navigation here. It’s a gamechanger, especially when coupled with newer ways modalities of intraoperative imaging.
It doesn’t take away the difficulties in indentifying problems of the craniovertebral junction or planning an appropriate treatment strategy. But it does make the surgeons life a little easier and reduces the risk of a malpositioned screw.
There have been vast tomes on CVJ abnormalities and their treatment, surgical strategies and it is impossible to break them all down in a single post. Or even 10. But head over to instagram. Comment and let me know what else you would like to read about. Next up though… rest of the cervical spine.